ENQUIRY FORM
Diabetic Eye Disease
If I have diabetes, why should I undergo an eye exam?
Diabetes affects one in ten Singaporeans and Asians. 20% of people with diabetes may develop diabetic retinopathy (affecting the retina or back surface of the eye), which is the second most common cause of blindness after age-related macular degeneration in developed countries. However, unlike age-related macular degeneration, diabetic blindness is largely preventable through regular screening.
Additionally, cataract and glaucoma are more common in diabetics than non-diabetics. Early detection through regular screening is key to preserving vision.
How often should I have my diabetic eye screening?
An annual eye screening is required upon diagnosis of diabetes. In the early stages of diabetic retinopathy, vision is not affected. However in the later stages, blurring of vision may occur.
What does the screening involve?
Vision testing, cataract assessment, eye pressure measurements and optic nerve assessment (to exclude diabetic-related glaucoma) and a dilated eye examination with retinal photography (to exclude diabetic retinal disease).
If diabetic retinopathy related retinal swelling is seen, our state of the art Zeiss™ Cirrus Optical Coherence Tomography can further delineate, in high-definition, images of the swelling.
What happens if I have been diagnosed with diabetic retinopathy?
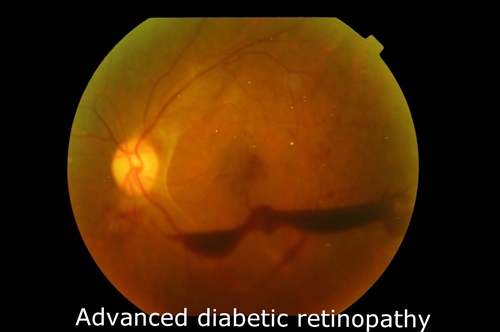
Diabetic retinopathy is graded into several stages from mild to severe.

Medical management includes control of blood sugars, blood pressure and cholesterol levels as well as lifestyle modification.
However, the mainstay of diabetic retinopathy treatment is laser photocoagulation for the severe stages. Our clinic offers the latest and most advanced treatment using the Topcon Pascal® laser for safe and precise treatment.
Eye surgery is occasionally required in very advanced stages.
In selected cases, eye injections of Lucentis® (ranibizumab), Eyelea® (aflibercept) or Avastin® (bevacizumab) may improve vision if the retinopathy affects the macula (central retina) and causes a decline in vision.

